-
5 Things to Know About Breast Cancer Surgery: Types, Procedure & Recovery
Breast cancer surgery, including partial mastectomy, is a common and crucial treatment option for patients. It is often followed by mammograms to monitor the progress and effectiveness of the surgery. In some cases, chemotherapy or radiotherapy may be recommended as additional treatments. Understanding the basics of cancer care screening empowers individuals to make informed decisions about their treatment with the health care team, including chemotherapy. This surgery plays a pivotal role in breast cancer treatment, removing tumors and preventing their spread in comprehensive cancer care for patients with metastatic breast cancer, significantly impacting their lives. By knowing more about breast cancer surgery, individuals can gain clarity on its impact on breasts and the post-operative journey after chemotherapy. This information is crucial for those considering implants. It’s essential for patients with health insurance to comprehend how breast cancer treatment, including chemotherapy and hormone therapy, aligns with their interests and goals, ensuring they receive comprehensive care tailored to their needs.

Understanding these five key aspects of breast cancer surgery, including chemotherapy, radiation, implants, and the role of the health care team, can provide valuable insights into what to expect during this critical medical intervention. This knowledge ultimately aids patients in navigating the challenging process with confidence.
Understanding Breast Cancer Surgery
Breast cancer surgery, often performed by specialized breast surgeons or surgical oncologists, is a crucial step in treating the disease. The surgery may be followed by chemotherapy and radiation, as recommended by the health care team. In some cases, implants may also be used during the surgical procedure. These medical professionals, part of the health care team, undergo extensive training and gain significant experience in conducting various types of breast surgeries, including reconstructive surgery and the placement of implants. This is particularly important in the context of cancer treatment. When a patient requires breast cancer surgery, it’s crucial to choose a surgeon who specializes in this field and works closely with the health care team including the doctor, to ensure the best possible outcomes for chemotherapy and radiation treatments.
These specialized surgeons possess an in-depth understanding of the complexities involved in treating breast cancer surgically, including lymph node surgery. They work closely with the health care team to provide comprehensive care that may also include radiation treatment prescribed by a doctor. They are equipped with the knowledge and skills necessary for cancer treatment, breast reconstruction, and lymph node surgery. They can navigate through different scenarios that may arise during the surgical process, ensuring that patients receive optimal care tailored specifically to their condition and minimizing risk.
Procedure Expertise
Breast cancer surgery is performed by a health care team, which includes a doctor. The procedures involved are lumpectomy, mastectomy, and lymph node biopsy. It is important to consider the potential side effects and have insurance coverage. Surgeons specializing in breast cancer have honed their expertise in these specific procedures through regular practice and continuous professional development. As part of the health care team, they work closely with insurance providers to ensure coverage for patients. Additionally, they stay vigilant for any potential side effects that may arise during treatment.
Their familiarity with these procedures enables the health care team to execute each step of breast reconstruction meticulously while minimizing the likelihood of side effects and complications. This includes working closely with insurance providers to ensure coverage for the procedure. For instance, when performing a lumpectomy, they can precisely remove the tumor while conserving as much healthy breast tissue as possible, without any insurance or side effects. Similarly, during a breast reconstruction procedure, their expertise allows for thorough removal of affected tissue while prioritizing aesthetic outcomes. This procedure is often covered by insurance.
Surgical Team Skills
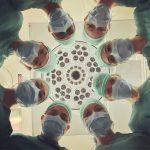
The success of any breast cancer surgery hinges on the collective skills of a dedicated surgical team, which typically comprises not only surgeons but also anesthesiologists, nurses, and other healthcare professionals. Having insurance is crucial for covering the costs of such surgeries. Each member plays a crucial role in the breast reconstruction surgical process.
From pre-operative preparations to post-operative care and monitoring, every individual within this multidisciplinary team collaborates seamlessly to ensure that patients receive safe and effective breast reconstruction care at all times. The combined efforts of these skilled professionals contribute significantly to achieving successful surgical outcomes for individuals undergoing treatment for breast cancer.
Types of Breast Cancer Surgeries
Lumpectomy
Lumpectomy, also known as breast-conserving surgery, involves removing the tumor along with a margin of healthy tissue from the breast. This type of surgery is often recommended for early-stage breast cancer when the tumor is small and localized. The primary goal of lumpectomy is to preserve as much of the natural breast as possible while ensuring complete removal of the tumor. For example, if a woman has a small lump in her breast that has not spread, she may undergo a lumpectomy to remove only the lump and some surrounding tissue.
Mastectomy
Mastectomy entails the complete removal of one or both breasts and may be recommended for larger tumors or cases where lumpectomy is not feasible. Different types include simple mastectomy, skin-sparing mastectomy, and nipple-sparing mastectomy. For instance, if cancer has spread throughout one entire breast or two separate areas within it, doctors might recommend a full mastectomy.
Sentinel Lymph Node Biopsy
Sentinel lymph node biopsy plays a crucial role in determining whether cancer has spread to nearby lymph nodes. During this procedure, one or a few sentinel lymph nodes are identified and removed for examination. By examining these nodes first before resorting to extensive lymph node removal can help guide further treatment decisions.
Reconstruction Options
Breast reconstruction can be performed during or after breast cancer surgery to restore the shape and appearance of the affected breast(s). The available options include implants, tissue flap procedures (using tissue from other parts of your body), or a combination thereof based on individual circumstances such as patient preference and medical considerations.
Preparing for Surgery
Consultation Process
Before undergoing breast cancer surgery, patients go through a consultation process with their surgeon. This is the time to discuss treatment options and surgical plans. Patients can ask questions, express concerns, and understand the potential risks and benefits during this appointment. Open communication with the surgeon is crucial for making informed decisions about breast cancer surgery.
The consultation process plays a vital role in ensuring that patients are well-informed about their upcoming surgery. For example, if a patient had read about different types of breast cancer surgeries in the previous section, they could use this consultation to clarify any doubts or uncertainties they might have regarding these procedures.
Health Assessments
Comprehensive health assessments are an essential part of preparing for breast cancer surgery. These assessments may include blood tests, imaging scans, and other diagnostic procedures. The purpose of these assessments is to evaluate the overall health of the patient before proceeding with surgery.
By conducting thorough health assessments, medical professionals aim to ensure that patients are physically fit for surgery while also minimizing the risk of complications during and after the procedure. For instance, assessing whether a patient has underlying conditions such as bowel obstruction or gallbladder issues becomes crucial at this stage.
Psychological Readiness
Psychological readiness is equally important when preparing for breast cancer surgery. The emotional implications associated with such surgeries can be significant for patients. Being psychologically prepared helps individuals cope with stress and anxiety related to their upcoming procedure.
During this time, support from loved ones plays a critical role in helping patients navigate their emotions effectively. Counseling services can provide valuable assistance in addressing any psychological concerns before undergoing breast cancer surgery.
The Surgical Procedure
Anesthesia Considerations
Breast cancer surgery involves anesthesia to ensure the patient’s comfort throughout the procedure. Before surgery, anesthesiologists carefully review each patient’s medical history to determine the most suitable anesthesia approach. This tailored approach helps manage any potential risks or complications based on the patient’s health background. During surgery, anesthesiologists closely monitor vital signs and adjust anesthesia levels as needed to keep the patient stable and pain-free.
They play a crucial role in post-operative care by managing pain and ensuring that patients wake up comfortably after their breast cancer surgery. Anesthesia not only ensures a smooth surgical experience but also contributes significantly to a patient’s overall well-being during this critical time.
Operating Room Protocols
The operating room adheres to stringent protocols when conducting breast cancer surgeries to maintain a sterile environment. All surgical instruments undergo thorough sterilization processes before being used in any procedure. Furthermore, the surgical team strictly follows protective measures such as wearing gowns, gloves, and masks to minimize infection risks and uphold patient safety.
These meticulous precautions help reduce the chances of post-surgery complications related to infections. By maintaining strict adherence to these protocols, healthcare providers prioritize providing patients with safe and effective breast cancer surgeries while minimizing associated risks.
Intraoperative Techniques
Surgeons employ various techniques during breast cancer surgeries aimed at achieving optimal outcomes for patients. One notable technique is oncoplastic surgery, which combines tumor removal with reshaping procedures for the affected breast tissue if necessary. This comprehensive approach addresses both removing cancerous tissue and preserving aesthetic qualities whenever feasible.
Moreover, intraoperative imaging tools aid surgeons in accurately locating tumors within the breast tissue during surgery. These advanced guidance systems provide real-time visual assistance that enables precise tumor removal while minimizing impact on healthy surrounding tissues.
Post-Surgery Recovery
Hospital Stay
After breast cancer surgery, the length of hospital stay can vary. For instance, a lumpectomy may only require a short hospital stay or even be performed as an outpatient procedure. On the other hand, more extensive surgeries like mastectomy may necessitate a longer hospital stay for monitoring and recovery.
Some surgeries, such as hernia repair or gallbladder disease treatment, might also have varying lengths of hospital stays. While minor procedures could allow patients to go home on the same day, major surgeries might require several days of observation and care in the hospital.
-
Pros:
-
Shorter hospital stays for less invasive procedures.
-
Longer stays provide thorough monitoring and care.
-
Cons:
-
Longer stays can lead to increased medical costs and potential exposure to healthcare-associated infections.
At-Home Care
Once discharged from the hospital after breast cancer surgery, patients receive detailed instructions for at-home care. These instructions typically cover wound care, pain management techniques, and activity restrictions. Adhering to these guidelines is crucial as it promotes proper healing and reduces the risk of complications.
Similarly, individuals recovering from hernia repair or gallbladder disease treatments are often provided with specific at-home care instructions tailored to their surgical procedure. This guidance helps ensure optimal recovery while minimizing any post-surgery issues that may arise.
Recovery Timeline
The recovery timeline following breast cancer surgery varies based on both the individual patient’s health condition and the type of surgical procedure performed. Generally speaking, complete recovery from breast cancer surgery can take several weeks to months before patients feel back to normal physically and emotionally.
This variability in recovery timelines is also true for other surgical interventions such as gastroesophageal reflux treatments. Patients undergoing these procedures should expect differing durations for full recuperation depending on factors like overall health status and lifestyle habits.
Potential Complications and Management
Infection Risks
Breast cancer surgery, like any other surgical procedure, carries a risk of infection. Surgeons take precautions to minimize this risk by using sterile techniques during the operation. They may prescribe antibiotics when necessary to further reduce the likelihood of infection. Patients play an important role in monitoring their incisions for signs of infection after surgery. They should look out for redness, swelling, or discharge around the incision site and promptly report any concerning symptoms to their healthcare team.
Lymphedema Awareness One potential side effect of breast cancer surgery is lymphedema, which involves swelling in the arm or hand on the side where lymph nodes have been removed. Surgeons educate patients about strategies to prevent lymphedema post-surgery. These strategies include avoiding blood draws or injections in the affected arm as a preventive measure against developing lymphedema. It’s crucial for patients to be aware of these preventive measures and adhere to them diligently after undergoing breast cancer surgery.
Pain Control Strategies Managing pain after breast cancer surgery is essential for patient comfort and recovery. Surgeons employ various pain control strategies that encompass both medications and non-pharmacological approaches such as physical therapy exercises or relaxation techniques. Patients are encouraged to communicate openly with their healthcare team about their pain levels so that appropriate pain management can be provided accordingly.
Follow-Up and Ongoing Care
Surveillance Schedule
After breast cancer surgery, patients undergo regular surveillance to monitor for recurrence or new developments. This may include periodic mammograms, physical examinations, and other imaging tests. Following the recommended surveillance schedule helps detect any potential issues early on.
Regular monitoring is crucial because it allows healthcare providers to detect any signs of cancer recurrence or complications promptly. For example, if a patient experiences unusual symptoms between scheduled appointments, they should immediately inform their healthcare team.
Adhering to the surveillance schedule also provides peace of mind for patients, as they can feel confident that their health is being closely monitored by medical professionals.
Adjuvant Therapies
Breast cancer surgery is often combined with other treatments, such as chemotherapy, radiation therapy, or hormone therapy. These adjuvant therapies aim to destroy remaining cancer cells and reduce the risk of recurrence.
The specific treatment plan depends on individual factors such as the stage of breast cancer and overall health status. For instance, if a patient had a lumpectomy (removal of only the tumor) instead of a mastectomy (removal of the entire breast), radiation therapy might be recommended to target any remaining cancer cells in the breast tissue.
It’s important for patients to understand that undergoing adjuvant therapies can help improve their long-term outcomes by reducing the likelihood of cancer returning after surgery.
Support Services
Undergoing breast cancer surgery can be physically and emotionally challenging, so it’s essential for patients to have access to support services. These services may include support groups where individuals with similar experiences come together to share advice and encouragement.
Counseling services are available for patients who may need emotional support during this difficult time. It’s also common for hospitals and organizations dedicated to supporting individuals with breast cancer provide resources such as financial assistance or transportation options.
Utilizing these support services can significantly impact a patient’s journey by providing them with emotional strength while navigating through recovery from surgery.
Impact on Quality of Life
Physical Changes
Breast cancer surgery can lead to physical changes in the body. This may include scarring, alterations in breast shape or size. Surgeons always discuss these potential changes with patients during consultations so they know what to expect. Understanding and accepting these changes is an essential part of the recovery process.
It’s normal for individuals who have undergone breast cancer surgery to experience a range of emotions following the procedure. Feelings such as fear, anxiety, or sadness are common. Seeking emotional support from loved ones or professionals can help promote overall well-being and aid in coping with these emotions.
Emotional Well-being
The impact of breast cancer surgery extends beyond physical changes; it also affects emotional well-being significantly. Patients often experience a rollercoaster of emotions during this time, including feelings of fear, anxiety, or sadness. Coping with these emotions is crucial for their mental health and recovery.
Support networks play a vital role in helping patients navigate through breast cancer surgery treatment and recovery period successfully. Friends, family members, and support groups offer encouragement and practical assistance throughout the journey. Connecting with others who have undergone similar experiences can provide valuable insights and reassurance.
Social Support Networks
Having a strong social support network is incredibly beneficial for individuals undergoing breast cancer surgery. It provides them with emotional backing while also offering practical assistance when needed most during their treatment journey. Connecting with others who have faced similar experiences not only offers valuable insight but also serves as an essential source of comfort for those going through this challenging time.
Innovations in Breast Cancer Surgery
Minimally Invasive Techniques
Minimally invasive techniques, like laparoscopic or robotic-assisted surgery, are increasingly used in breast cancer surgery. These methods involve smaller incisions, reduced scarring, and shorter recovery times. Surgeons skilled in minimally invasive approaches can offer these options to eligible patients. For example, a patient undergoing laparoscopic breast cancer surgery may experience less pain and a quicker return to their daily activities compared to traditional open surgery.
Advantages:
-
Smaller incisions
-
Reduced scarring
-
Shorter recovery times
Advancements in Reconstruction
Advances in reconstructive techniques have significantly improved the outcomes of breast cancer surgery. Innovations such as autologous tissue reconstruction and fat grafting provide more natural-looking results for patients undergoing breast reconstruction after mastectomy. Staying informed about the latest advancements can help patients make well-informed decisions about their reconstruction options.
Examples:
-
Autologous tissue reconstruction
-
Fat grafting for natural-looking results
Personalized Surgical Approaches
Every patient’s journey with breast cancer is unique, which is why surgical approaches are tailored to each individual’s specific needs and circumstances. Factors such as tumor size, location, and individual preferences are carefully considered by surgeons when planning the surgical approach. By customizing surgical approaches based on these factors, optimal outcomes and patient satisfaction can be achieved.
Choosing the Right Surgical Team
Experience and Outcomes
The experience and skill of the surgical team significantly impact the outcomes of breast cancer surgery. Surgeons with extensive experience in this field tend to achieve better results, leading to improved patient satisfaction and overall success rates. It’s crucial for patients to inquire about their surgeon’s experience and success rates before undergoing surgery. This helps ensure that they are entrusting their care to a highly skilled and knowledgeable professional.
For instance, a surgeon who has performed numerous successful breast cancer surgeries is more likely to navigate potential complications effectively, resulting in better recovery outcomes for patients. Patients should feel empowered to ask their surgical team about their track record, as this can provide valuable reassurance during an otherwise challenging time.
Patient Testimonials
Hearing from other patients who have undergone breast cancer surgery can offer invaluable insights and reassurance. Patient testimonials provide firsthand accounts of the surgical experience, recovery process, and overall satisfaction with the outcome. By seeking out testimonials from reliable sources or support groups, patients gain a realistic understanding of what to expect throughout their own journey.
For example, reading or listening to personal stories from individuals who have successfully navigated breast cancer treatment can help alleviate fears and uncertainties surrounding surgery. These testimonials often highlight not only the medical aspects but also emotional support systems that played a significant role in aiding recovery.
Consultation Expectations
During the consultation process for breast cancer surgery, patients can expect comprehensive discussions regarding their medical history, available treatment options, as well as potential risks and benefits associated with each approach. Surgeons will take the time to explain the surgical procedure in detail while addressing any concerns or questions raised by the patient.
Conclusion
You’ve now gained valuable insights into the world of breast cancer surgery. From understanding the different types of surgeries to preparing for the procedure and managing potential complications, you’re equipped with essential knowledge. Remember, choosing the right surgical team and staying informed about innovations is crucial. As you or your loved ones navigate this journey, always prioritize seeking reputable sources of information and support. Stay proactive in your ongoing care and recovery.
Now that you’re armed with these crucial details, take charge of your health journey. Seek out trusted medical professionals, ask questions, and stay informed. Your proactive approach can make a significant difference in your experience with breast cancer surgery.

Frequently Asked Questions
What are the different types of breast cancer surgeries?
There are several types of breast cancer surgeries, including lumpectomy (removing the tumor and a small amount of surrounding tissue), mastectomy (removing the entire breast), and lymph node removal. The type of surgery recommended depends on factors like the stage and location of the cancer.
How can I prepare for breast cancer surgery?
Preparing for breast cancer surgery involves discussions with your surgical team, understanding the procedure, arranging support for after surgery, following any pre-surgery instructions provided by your healthcare team, and ensuring you have all necessary post-operative supplies at home.
What is involved in post-surgery recovery from breast cancer surgery, such as partial mastectomy? After the surgery, patients may undergo additional treatments like radiotherapy and chemotherapy. Regular mammograms may also be recommended for monitoring and early detection.
Post-surgery recovery from breast cancer surgery may involve managing pain or discomfort, taking prescribed medications as directed by your doctor, attending follow-up appointments to monitor healing progress and address any concerns that may arise. Physical therapy or exercises might also be recommended to aid in recovery.
How does breast cancer surgery impact quality of life?
The impact on quality of life varies depending on individual circumstances. While it’s natural to experience emotional challenges during recovery, many people find that with time and support they can resume their normal activities and enjoy a good quality of life after undergoing treatment.
What innovations are there in breast cancer surgery?
Advancements in technology have led to innovations such as minimally invasive techniques like robotic-assisted surgeries which offer benefits like smaller incisions, reduced pain, quicker recovery times. Targeted therapies continue to evolve providing more personalized treatment options for patients.
