Sentinel lymph Node
Sentinel lymph Node
The sentinel lymph node, a pivotal player in cancer staging and treatment, holds a significant role in detecting the spread of cancerous cells. This key node, along with nearby lymph nodes, serves as sentinel nodes, guiding the health care team of medical professionals and surgeon to determine the extent of disease progression and plan appropriate interventions. By identifying the sentinel lymph node, healthcare providers can make informed decisions that impact patient outcomes positively. Understanding the importance of this primary node in the lymphatic system is essential for individuals navigating through cancer diagnoses and treatments.
Sentinel Lymph Node Basics
Anatomy Insights
The sentinel lymph node is typically located closest to the primary tumor site in the body. It acts as a crucial checkpoint in the lymphatic system, filtering harmful substances and cancer cells. This sentinel node plays a vital role in monitoring and responding to potential threats within the body.
Pathophysiological Aspects
In disease progression, cancer cells have the potential to spread to sentinel lymph nodes (slnb), indicating possible metastasis. Understanding the pathophysiology of these nodes is essential for early detection and treatment planning. Sentinel lymph nodes also play a pivotal role in triggering an immune response against foreign invaders.
Clinical Implications
Identifying and evaluating sentinel lymph nodes (slnb) hold significant clinical importance in various medical fields. These nodes serve as key indicators for staging different diseases, guiding treatment decisions. The status of sentinel lymph nodes often determines the prognosis and overall outcome for patients undergoing treatment.
Why Sentinel Biopsy
Diagnostic Purpose
Sentinel lymph node biopsy plays a crucial role in diagnosing cancer by identifying the first lymph node where cancer is likely to spread. This procedure helps determine the stage of cancer and whether it has metastasized to other parts of the body. The accurate evaluation of sentinel lymph nodes is essential for providing precise information about the spread of cancer.
Understanding the importance of accurately identifying and evaluating sentinel lymph nodes is vital as they serve as indicators for potential cancer spread. By analyzing these nodes, healthcare professionals can make informed decisions regarding further treatment options. Utilizing sentinel lymph nodes for diagnostic purposes allows for targeted treatment, minimizing unnecessary procedures and reducing complications.
Precisely identifies potential spread
Guides treatment decisions effectively
Reduces unnecessary procedures and complications
Treatment Planning
Information obtained from evaluating sentinel lymph nodes significantly influences treatment planning by providing insights into the extent of cancer spread. These nodes help determine whether additional treatments such as chemotherapy or radiation therapy are necessary. The status of sentinel lymph nodes aids in deciding the appropriate course of action, ensuring tailored treatment plans for each patient.
The role of sentinel lymph nodes in determining the extent of surgery or other treatments cannot be overstated, as it directly impacts patient outcomes. By assessing these key nodes, medical professionals can develop personalized treatment strategies that address individual needs effectively. Understanding the status of sentinel lymph nodes enables healthcare providers to offer targeted therapies that optimize patient care.
Influences treatment decisions
Determines extent of additional treatments
Guides personalized treatment strategies
Lymph Node Clusters
Key Locations
Sentinel lymph nodes are commonly found in areas such as the armpit, groin, and neck. These sentinel nodes, lymph node clusters, act as primary locations for initial cancer spread detection. The precise mapping of sentinel lymph nodes is crucial for accurate diagnosis and treatment planning.
Different types of cancer can lead to variations in sentinel lymph node locations. For instance, breast cancer often involves the axillary lymph nodes in the armpit region. Melanoma, on the other hand, may affect lymph nodes near the primary tumor site. Understanding these variations is essential for effective disease management.
The importance of accurately identifying and evaluating sentinel lymph node locations cannot be overstated. By pinpointing these key locations, medical professionals can determine the extent of cancer spread and tailor treatment strategies accordingly. This targeted approach enhances patient outcomes and reduces unnecessary interventions.
Involvement in Diseases
Sentinel lymph nodes play a critical role in various diseases, particularly cancer. These sentinel nodes, key lymph node clusters, serve as early indicators of cancer spread, guiding treatment decisions. Evaluating sentinel lymph nodes helps physicians assess disease progression and formulate personalized care plans.
In disease management, the evaluation of sentinel lymph nodes is pivotal. By analyzing these primary sites of metastasis, healthcare providers can determine the stage of cancer and plan appropriate interventions. Timely identification and assessment of sentinel lymph nodes significantly impact patient prognosis and quality of life.
As indicators of disease progression, sentinel lymph nodes offer valuable insights into the spread and aggressiveness of cancer. Monitoring changes in these key locations allows healthcare professionals to adjust treatment strategies accordingly. The evaluation of sentinel lymph nodes remains a cornerstone in oncology for predicting outcomes and optimizing patient care.
Preparing for Biopsy
Pre-Procedure Steps
Before a sentinel lymph node biopsy, patients need to undergo several essential pre-procedure steps. Firstly, they must follow specific instructions provided by their healthcare provider, usually involving fasting before the procedure. This ensures accurate results and minimizes potential complications. Patient preparation also includes discussing any allergies or medications with the medical team to prevent adverse reactions during the biopsy.
Informed consent plays a crucial role in the sentinel lymph node biopsy process. Patients must understand the procedure’s purpose, risks, and benefits before providing consent. Pre-procedural assessments such as blood tests and imaging scans are conducted to evaluate the patient’s overall health status and identify any potential issues that may affect the biopsy’s outcome.
Patient Consultation
Patient consultation is a vital aspect of preparing for a sentinel lymph node biopsy. Clear communication between the healthcare provider and the patient is key to ensuring that the patient understands the procedure, its significance, and potential outcomes. During the consultation, patients have the opportunity to ask questions and express any concerns they may have about the biopsy.
Addressing patient concerns during sentinel lymph node biopsy consultations helps alleviate anxiety and build trust between the patient and medical team. Patients may inquire about post-biopsy care, recovery time, or potential side effects of the procedure. By addressing these questions comprehensively, healthcare providers can ensure that patients feel informed and confident about undergoing a sentinel lymph node biopsy.
Biopsy Procedure
Before Biopsy
Before undergoing a sentinel lymph node biopsy, patients need to follow specific preparations. These include dietary adjustments, medication changes, and other pre-biopsy considerations. Strictly adhering to these instructions is crucial for optimal biopsy results.
Patients are typically advised to follow dietary restrictions before the procedure. They may need to avoid certain foods or beverages to ensure accurate test results. Medication adjustments might also be necessary to prevent any interference with the biopsy process. Following these guidelines is essential for a successful biopsy outcome.
To achieve accurate results during a sentinel lymph node biopsy, patients must adhere to all pre-biopsy instructions diligently. Any deviations from the recommended preparations could affect the accuracy of the procedure and potentially lead to complications.
During Biopsy
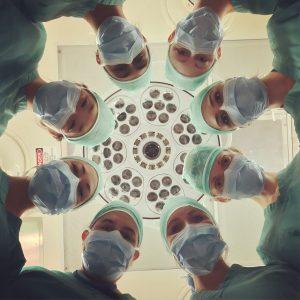
During a sentinel lymph node biopsy, surgeons perform a surgical procedure involving a small incision in the targeted area. The surgeon uses techniques such as injecting dye to locate and extract the sentinel lymph node accurately. Precision and accuracy are critical during this process to ensure the correct identification of the sentinel lymph node.
The surgical team meticulously locates and removes the sentinel lymph node using specialized techniques. By conducting the procedure with precision, surgeons can minimize potential risks and complications associated with the biopsy. Ensuring accuracy throughout the process is vital for obtaining reliable results.
After Biopsy
After a sentinel lymph node biopsy, patients receive post-biopsy care instructions that are crucial for their recovery. It is important for patients to follow these guidelines carefully to promote healing and reduce the risk of complications. Monitoring for any signs of infection or adverse reactions is essential after the procedure.
Patients should be aware of potential side effects or complications that may arise following a sentinel lymph node biopsy. These could include pain, swelling, or infection at the incision site. Promptly reporting any unusual symptoms to healthcare providers is important for timely intervention and management.
Risks and Complications
Common Risks
Sentinel lymph node biopsy carries potential complications such as infection, bleeding, or nerve damage. These risks are inherent to any surgical procedure and require careful consideration. Informed consent is crucial before undergoing the biopsy to understand and acknowledge these risks. Patients should be aware of the possibility of side effects post-procedure.
Complications like infections can arise due to the introduction of foreign instruments into the body during the biopsy. Bleeding is another risk that can occur, especially in individuals with underlying clotting disorders. Nerve damage is a rare but serious complication that may lead to sensory or motor deficits in the affected area. Therefore, a thorough risk assessment is essential prior to proceeding with the sentinel lymph node evaluation.
Lymphedema Understanding
Lymphedema refers to swelling caused by a blockage in the lymphatic system, commonly observed after lymph node removal surgeries like sentinel lymph node biopsy. The procedure involves identifying and removing specific lymph nodes, disrupting the normal flow of lymph fluid in the body. This disruption can increase the risk of developing lymphedema in some patients.
The evaluation of sentinel lymph nodes plays a critical role in determining cancer spread without removing excessive nodes, reducing the risk of lymphedema development compared to traditional lymph node dissection methods. To manage and prevent lymphedema post-biopsy, patients are advised to engage in physical therapy, wear compression garments, and practice proper limb care techniques. Early detection and intervention are key in minimizing the impact of lymphedema on patients’ quality of life.
Expected Results
Interpretation Guidelines
Interpreting sentinel lymph node biopsy results requires a keen eye for detail. Healthcare providers analyze the appearance, size, and texture of the lymph nodes. Different signs such as color changes or abnormal shapes may indicate potential issues. It is crucial to identify any irregularities promptly.
Understanding the implications of various findings is essential for patient care. Positive results may necessitate further testing or treatment adjustments. Conversely, negative results provide reassurance and guide next steps in the treatment plan. Accurate interpretation plays a pivotal role in ensuring optimal outcomes for patients undergoing biopsy procedures.
Follow-Up Care
After a sentinel lymph node biopsy, diligent follow-up care is imperative. Patients need close monitoring to detect any complications early on. Regular check-ups and imaging tests help track recovery progress and ensure no adverse effects arise from the procedure. Healthcare providers play a vital role in providing guidance and support throughout the post-biopsy journey.
It is recommended to adhere to a structured follow-up schedule post-biopsy. This schedule typically includes frequent visits initially, gradually spacing them out as the patient recovers. Monitoring procedures involve physical examinations, imaging studies, and laboratory tests to assess overall health status accurately. Consistent follow-up care enhances patient well-being and aids in addressing any arising concerns promptly.
Clinical Trials Insight
Ongoing Research
Recent research on sentinel lymph nodes focuses on enhancing detection accuracy and minimizing invasiveness. Studies are investigating novel imaging techniques like fluorescent dyes to improve identification during surgery. Researchers are exploring the use of molecular markers to identify cancer cells more precisely.
Advancements in technology have led to the development of innovative tools such as handheld gamma probes for real-time tracking of sentinel lymph nodes. These advancements aim to streamline the evaluation process and reduce the risk of false negatives, ultimately improving patient outcomes.
Researchers are also investigating the potential role of artificial intelligence (AI) in analyzing imaging data for sentinel lymph node evaluation. By leveraging AI algorithms, healthcare providers may achieve faster and more accurate interpretations of imaging results, leading to better decision-making in clinical practice.
Future Directions
The future of sentinel lymph node evaluation is poised for significant progress, with a focus on personalized medicine approaches tailored to individual patient needs. Advancements in precision medicine may enable targeted therapies based on specific characteristics of sentinel lymph nodes, optimizing treatment outcomes.
Innovations such as nanotechnology hold promise for enhancing the sensitivity and specificity of sentinel lymph node procedures. Nanoparticles can be engineered to target cancer cells specifically, offering a highly precise method for detecting and treating metastases in sentinel lymph nodes.
The integration of multimodal imaging techniques, combining different imaging modalities like ultrasound and MRI, is expected to revolutionize sentinel lymph node evaluation. This integrated approach could provide comprehensive insights into nodal status, guiding clinicians in making informed decisions regarding further treatment strategies.
Patient Support Resources
Education Materials
Patient education and awareness are crucial for individuals undergoing sentinel lymph node evaluation. Providing resources and educational materials can help patients understand the procedure better. Reliable sources of information play a key role in empowering patients with knowledge about sentinel lymph nodes.
Supporting materials such as brochures, videos, and online articles can explain the evaluation process in simple terms. Patients benefit from knowing what to expect during the procedure and its significance in cancer staging. Educational materials also address common concerns and questions that patients may have.
Leading medical institutions often offer comprehensive guides on sentinel lymph node evaluation. These resources outline the procedure, potential risks, and post-evaluation care instructions. Patients can access these materials to gain insights into their diagnosis and treatment journey effectively.
Support Networks
Support networks and organizations play a vital role in assisting patients with sentinel lymph node-related concerns. Connecting with support groups offers emotional and practical assistance to individuals navigating through the evaluation process. These networks provide a sense of community and understanding for patients facing similar challenges.
Patients find solace in sharing their experiences with others who have undergone sentinel lymph node evaluation. Support groups create a safe space for individuals to express their fears, hopes, and uncertainties regarding the procedure. Building connections within these networks can alleviate feelings of isolation and anxiety.
Engaging with support networks not only benefits patients but also extends support to their families. Caregivers often find comfort in connecting with other families going through similar experiences. These networks foster a supportive environment where both patients and their loved ones receive encouragement and guidance.
Closing Thoughts
You have now gained a comprehensive understanding of sentinel lymph nodes, their significance in biopsies, and what to expect during the procedure. By being informed about lymph node clusters, biopsy preparation, potential risks, and expected outcomes, you are better equipped to navigate this aspect of your healthcare journey. Remember that clinical trials offer valuable insights and patient support resources can provide additional assistance and guidance.
Take charge of your health by staying informed and proactive. If you have concerns or questions about sentinel lymph node biopsies, don’t hesitate to reach out to your healthcare provider for clarification. Your well-being is paramount, and being knowledgeable about these procedures empowers you to make informed decisions regarding your health. Stay engaged, stay informed, and prioritize your health above all else.
Frequently Asked Questions
What is a sentinel lymph node?
A sentinel lymph node is the first lymph node where cancer cells are most likely to spread from a primary tumor. Identifying and examining this node can help determine if cancer has spread beyond the original site.
How does a sentinel biopsy help in cancer diagnosis?
A sentinel biopsy helps in identifying whether cancer has spread to the lymph nodes, aiding in staging and treatment decisions. By analyzing the sentinel node, doctors can assess the extent of disease without needing to remove multiple nodes.
What are lymph node clusters?
Lymph node clusters are groups of small, bean-shaped structures that act as filters for harmful substances. They play a crucial role in the immune system by trapping and destroying pathogens. Understanding their location and function is vital in cancer diagnosis and treatment planning.
How should one prepare for a sentinel biopsy?
To prepare for a sentinel biopsy, patients may need to avoid eating or drinking before the procedure, inform their healthcare provider about medications, and follow specific instructions provided by their medical team. Proper preparation ensures accurate results and reduces risks during the biopsy.
What are the risks and complications associated with a sentinel biopsy performed by the surgeon and examined by the pathologist?
While generally safe, risks of a sentinel biopsy include infection, bleeding, allergic reactions to dyes used, nerve damage, or lymphedema. It’s essential to discuss potential complications with your healthcare provider before undergoing the procedure to make an informed decision.

 Sentinel Lymph Node Basics
Sentinel Lymph Node Basics